Miscellaneous
Miscellaneous  Miscellaneous
Miscellaneous  Our World
Our World 10 Green Practices That Actually Make a Difference
 Humans
Humans Ten Historic Men Who Deserve Way More Credit Than They Got
 Movies and TV
Movies and TV The 10 Most Heartwarming Moments in Pixar Films
 Travel
Travel Top 10 Religious Architectural Marvels
 Creepy
Creepy 10 Haunted Places in Alabama
 History
History Top 10 Tragic Facts about England’s 9 Days Queen
 Food
Food 10 Weird Foods Inspired by Your Favorite Movies
 Religion
Religion 10 Mind-Blowing Claims and Messages Hidden in the Bible Code
 Facts
Facts 10 Things You Never Knew about the History of Gambling
 Miscellaneous
Miscellaneous Ten Groundbreaking Tattoos with Fascinating Backstories
 Our World
Our World 10 Green Practices That Actually Make a Difference
 Humans
Humans Ten Historic Men Who Deserve Way More Credit Than They Got
Who's Behind Listverse?

Jamie Frater
Head Editor
Jamie founded Listverse due to an insatiable desire to share fascinating, obscure, and bizarre facts. He has been a guest speaker on numerous national radio and television stations and is a five time published author.
More About Us Movies and TV
Movies and TV The 10 Most Heartwarming Moments in Pixar Films
 Travel
Travel Top 10 Religious Architectural Marvels
 Creepy
Creepy 10 Haunted Places in Alabama
 History
History Top 10 Tragic Facts about England’s 9 Days Queen
 Food
Food 10 Weird Foods Inspired by Your Favorite Movies
 Religion
Religion 10 Mind-Blowing Claims and Messages Hidden in the Bible Code
 Facts
Facts 10 Things You Never Knew about the History of Gambling
10 Ways That Culture Affects Our Delusions
We may experience delusions (strong beliefs that conflict with rational evidence or reality) when our brains try to understand the distress we associate with mental illness. Many of us think that delusions are as individualized as our fingerprints. But the truth is that our brains shape our delusions from the technologies and cultures of our time.
Delusions go in and out of style, just like clothing and hairstyles. Delusions can be sold and even exported to us from other cultures. Unfortunately, we can’t always count on our doctors for guidance because they’re often as delusional as we are.
10Cultural Influences

Our cultures provide the background material to understand and tell our stories, including the narrative for our delusions. The people who treat us—whether doctors, priests, or shamans—also help to form our delusions by defining the symptoms of mental illness.
“We might think of the culture as possessing a ‘symptom repertoire‘—a range of physical symptoms available to the unconscious mind for the physical expression of psychological conflict,” medical historian Edward Shorter explained to the New York Times. “In some epochs, convulsions, the sudden inability to speak, or terrible leg pain may loom prominently in the repertoire. In other epochs, patients may draw chiefly upon such symptoms as abdominal pain, false estimates of body weight, and enervating weakness as metaphors for conveying psychic stress.”
For example, some Southeast Asian men may suffer from koro, the belief that their genitals are shrinking, even though there’s nothing wrong physically. In the Middle East, individuals with zar are believed to be possessed by spirits, which may cause attacks of shouting, laughing, and singing as part of their feelings of detachment.
Our mass delusions are influenced the same way. For example, repressed nuns suffered many mass delusions from the 15th to the 19th centuries. When combined with popular beliefs in demons, strict religious discipline often triggered hysterical fits in these women, including swearing, exposing and rubbing their genitals, and thrusting their hips as though having intercourse. Priests claimed to exorcise the demons, although some nuns were jailed or burned at the stake.
From the 18th through the early 20th centuries, extreme working conditions caused abnormal movements, convulsions, and neurological symptoms for groups of workers in Western factories.
As the 20th century progressed, mass delusions switched more to anxiety symptoms over environmental and war-related fears. After poison gas killed 90,000 people in World War I, Americans became obsessed with the fear of gas. In the early 1930s, dozens of people in rural Virginia were convinced that someone had sprayed harmful gas in their homes at night. After serious investigation, authorities found that the real sources ranged from passing flatulence to chimney flues that had stopped up.
Fear of anthrax after the 9/11 terror attacks also sparked many false alarms in the US population. For example, one student and teacher claimed to have chemical burns on their forearms after they opened a letter in October 2001. However, nothing unusual was found in the envelope.
9Technological Influences

Although the loneliness, alienation, and other anxieties that cause delusions aren’t new, the way they’re expressed varies over time to mirror cultural changes, including technology. Before the late 19th century, delusions of being controlled or persecuted usually centered on witchcraft and the supernatural. That changed when new technologies such as the telegraph, telephone, radio, TV, electricity, X-rays, lasers, and the Internet became popular.
People don’t usually go back in time with their delusions unless an earlier era is fixed in their minds for some reason. So delusions today are mainly about being controlled or persecuted through computers and the Internet, not through radio waves as in the 1940s.
One 2010 study showed that prolonged Internet use can trigger unexpected psychotic episodes. In three separate cases, women 30–50 years old with no serious psych issues developed delusions and hallucinations from using the Internet many hours every day. Each woman had been unhappy in a previous intimate relationship but was now involved in a strictly online relationship with a man. Over time, these women lost touch with reality. One of them believed she could feel her online love physically touching her, even though she’d never met him in person. All of the women required antipsychotic medications to stop their delusions and return to normal functioning.
In another case, a man was convinced that his computer was used to implant thoughts in his head and to poison him through his keyboard.
Long ago, new materials were the technologies of their time. For example, the glass delusion gained steam in Europe until it became especially popular in the 1600s. It seemed to start with French king Charles VI, who was paranoid about betrayal and assassination. At times, he would have spells where he wouldn’t move. Convinced he was made of glass, he was afraid he would break. He also wrapped his body in blankets to stop his buttocks from shattering. Some psychologists believe this represents a fear of fragility or social humiliation. In a rare case from the 1960s, a young man in the Netherlands told the BBC that people looked through him like glass in a window. “You [don’t see the glass in the window]. But it is there,” said the man. “That’s me. I’m there, and I’m not there. Like the glass in the window.”
8Media And Entertainment Influences
Whether or not the 1938 War of the Worlds radio broadcast by Orson Welles actually caused the panic and mass delusion that’s been alleged over the years, we have seen delusions shaped by topics in the media or entertainment.
In 2008, the first case of climate change delusion was reported by doctors in Australia. Believing the world faced almost certain eco-destruction, their patient, a young man of 17, wouldn’t drink water because he felt guilty that doing so would kill millions of people. Immediately, there was a public outcry, with some people accusing the media of causing this man’s delusion by sensationalizing climate change. One blog ran the headline “Al Gore Is Literally Driving People Crazy.” But we’ve already seen that people’s delusions are a way to express their anxieties using stories that reflect the times in which they live.
Entertainment also fuels a lot of delusions. Some people believe they’re characters in computer games. Others are convinced they have romantic relationships with or are being persecuted by popular stars.
The Truman Show Delusion (TSD), named after an American movie about a man who finds out that his entire life is a reality TV show, narrates old anxieties of persecution and control in a modern story. With so much of our lives recorded without our knowledge or permission, and so many people who want to be on reality shows, some people now have delusions that they’re starring in their own reality shows.
“[Patients feel] as though their family perhaps were reading from a script, there were cameras everywhere at all time[s], they had no privacy,” psychiatrist Dr. Joel Gold told NPR. “And this was obviously—for most—very, very disturbing. For a small minority, there was an excitement about it, that they were the most famous person on Earth. But eventually, even for those people, it became unbearable.”
Gold notes that TSD is unusual in at least one important way. While most delusions are focused on one unreal area of life, such as alien abduction, TSD encompasses the patient’s whole world. Nothing is real to them.
7The Export Of America’s Delusions

Ethan Watters argues in his book Crazy Like Us that the US has exported its approach toward mental illness to other countries. That happens even when American definitions of illness don’t fit the other culture’s symptoms.
Although one antibiotic may cure the same bacterial infection anywhere in the world, that approach may not work when treating mental illness. Watters questions if we’re helping or harming patients if we don’t recognize the different customs that define our delusions and treat them accordingly.
“This does not mean that these illnesses and the pain associated with them are not real, or that sufferers deliberately shape their symptoms to fit a certain cultural niche,” writes Watters. “It means that a mental illness is an illness of the mind and cannot be understood without understanding the ideas, habits, and predispositions—the idiosyncratic cultural trappings—of the mind that is its host.”
After the 2004 tsunami in Sri Lanka, American psych experts rushed to help. They assumed the Sri Lankans would exhibit symptoms of post-traumatic stress disorder (PTSD). But that was at odds with the native culture. “It was not the nightmares or flashbacks that most of the population was concerned with,” trauma expert Gaithri Fernando told the New York Times. “The deepest psychological wounds for Sri Lankans were not on the PTSD checklists; they were the loss of or the disturbance of one’s role in the group.”
Where Americans saw damage to the mind, Sri Lankans saw damage to their social groups. American psychology professor Ken Miller observed similar results in Afghanistan, Bosnia, and Guatemala. PTSD symptoms didn’t fit the war-related trauma that occurred in those countries. To export American psychiatry to certain countries, developed or not, may be as much of a cultural mismatch as sending Namibian witch doctors to treat American patients after the 9/11 terror attacks.
If anxiety about changes in the world produces delusions for some people, are American psychiatrists making the problem worse by insisting on changing the way other cultures define and cope with their stressors? As we’ll talk about shortly, American ideas of psychiatry don’t always equate to better treatments and outcomes for patients. They’re not always done in the best interests of the patient, either.
6The Doctors Who Diagnose Us Are Also Delusional

Some doctors may believe that they evaluate and treat mental illness objectively. That’s especially true of some US practitioners, who believe that other countries have cultural delusions but US doctors treat real brain diseases with a scientific approach.
However, US doctors are just as culture-bound and delusional in their approach to mental illness as everyone else. With all their expensive machines to view the brain and medications to alter brain chemistry, they simply don’t recognize it. As Ethan Watters writes, “All mental illnesses, including depression, PTSD and even schizophrenia, can be every bit as influenced by cultural beliefs and expectations today as hysterical-leg paralysis or the vapors or zar or any other mental illness ever experienced in the history of human madness.”
As we saw with Sri Lanka, Western doctors think they understand what life events trigger mental illness, and they’re convinced that they know how to treat it. Some American doctors also believe that it’s good to talk about personal traumas, analyze them, and vent emotionally. There’s a belief that we’re mentally fragile. But many cultures, including some in more developed countries like Australia, simply don’t share those views, which can make American treatments ineffective at best.
That’s not to say that the US hasn’t made any advances in treatment that would help patients in other countries. But it often seems that US doctors have closed their minds to alternative methods of dealing with mental illness.
5Better Outcomes In The Developing World

Beginning in the early 1970s, the World Health Organization (WHO) conducted three international studies of schizophrenia patients that lasted about 30 years in total. The results showed that the relapse rate for schizophrenics in Europe and the US was as much as 67 percent higher when compared to developing countries.
That led to widespread debate as to what happened. One theory is that schizophrenia patients are treated more kindly and are better kept within social groups in some developing countries. Anthropologist Juli McGruder studied schizophrenics and their families in Zanzibar, where people with delusions are believed to be possessed by spirits. “Muslim and Swahili spirits are not exorcised in the Christian sense of casting out demons,” McGruder told the New York Times. “Rather they are coaxed with food and goods, feted with song and dance. They are placated, settled, reduced in malfeasance.” The patient is seen as having a temporary illness, not a new identity. When the illness goes into remission, the patient can function in society again, at least for a while.
Meanwhile, Western cultures value control over self and circumstances to such a degree that mental illness directly opposes that view. Unlike developing countries that accept spirit possession, family members in Western cultures expect their loved ones to get better through force of will. Patients feel more isolated and are less likely to go back to work. Their mental illness is often seen as permanent.
Some researchers believe that the WHO studies were conducted incorrectly. They also feel that the outlook for schizophrenia patients in developing countries has worsened considerably in recent years. They’re calling for new research.
Other studies show that different medication usage accounted for the outcomes in the WHO studies. Those researchers concluded that limiting the use of antipsychotic drugs works better in the long run for schizophrenia patients in all countries.
Even so, none of the studies appeared to show that Western medicine produced clearly better results for their schizophrenia patients.
4The Sale Of Mental Illness

At least one reason the US is so intent on exporting its definitions and treatments of mental illness, including delusions, is drug company profits. One of the best examples happened in Japan at the turn of the 21st century, when drug companies convinced the Japanese public that they suffered from mild depression, which was called kokoro no kaze, or “cold of the soul.” Of course, drug companies provided expensive antidepressants as the cure.
Until then, the Japanese medical community had only dealt with major depressive disorders. With a suicide rate double that of the US, Japan obviously had mental health problems. The average length of a hospitalization for mental illness was around 390 days, far more than the US average of under 10 days. Officially, mild depression didn’t exist in Japan. But after the drug companies rolled out their media campaign, doctor visits for depression soared almost 50 percent in just four years.
”I could take you all over the world, and you would have no difficulty recognizing severely depressed people in completely different settings,” psychiatry professor Arthur Kleinman told the New York Times. “But mild depression is a totally different kettle of fish. It allows us to relabel as depression an enormous number of things.” It’s hard to know where moodiness ends and depression begins. So it’s quite possible that the Japanese began to define conditions that weren’t even diseases as mild depression. They were told repeatedly that drugs were the cure.
One 39-year-old man, Naoya Mitake, was put on different rounds of antidepressants for about two years to treat insomnia and fatigue. He had been convinced by drug company educational campaigns that his feelings had a chemical basis that could only be treated by drugs. But it never completely worked for him. Then he accidentally found his own cure: fasting.
As Japanese psychiatrist Yutaka Ono explained to the New York Times, “[The drug companies] ran a very intense campaign about mild depression where a beautiful young lady comes out all smiles and says, ‘I went to a doctor and now I’m happy.’ You know, depression is not that easy. And if it is that easy, it might not be depression.”
Still, antidepressant sales quintupled in Japan between 1998 and 2003, shortly after the marketing campaigns began.
3Our Relationship With Our Delusions
Stanford anthropologist Tanya Luhrmann examined the way patients with psychotic disorders interacted with the voices (auditory hallucinations) they heard as part of their conditions. In the US, voices were characterized as threatening and harsh. In Ghana and India, the voices were often considered benign, even playful.
Luhrmann thinks that American doctors should pay more attention to both auditory hallucinations and cultural differences in psychiatric diseases. “Our work found that people with serious psychotic disorder in different cultures have different voice-hearing experiences,” she said. “That suggests that the way people pay attention to their voices alters what they hear their voices say. That may have clinical implications.”
In a study of 60 adults with schizophrenia—20 each from Ghana, India, and the US—Luhrmann found that people in all three countries heard good and bad voices, whispering, and an unidentified source of hissing. However, the striking difference came in the interpretations of their experiences. All the US patients had negative experiences that they considered to be brain disease symptoms. They viewed voices as a hateful, violent bombardment. It often felt like war to them.
About half of the Indian patients heard relatives advising them to complete tasks. Sometimes, they interpreted the voices as playful or entertaining. Most of them did not describe their hallucinations as part of a brain disease. The same was true for the Ghanaian patients. In their culture, it’s believed that spirits can talk, so they didn’t characterize voices as a psych problem. Half of them reported their experiences in a positive manner. Plus, 80 percent thought they had heard from God.
Luhrmann believes these different reactions reflect the patients’ cultures. Americans value independence, individuality, and control, but Ghanaians and Indians define themselves through their relationships with other people. This suggests beneficial new approaches to treating schizophrenia, such as naming patients’ voices and forging relationships with them.
“The problem is not hearing voices,” Dr. Marius Romme, founder of advocacy group Intervoice, told The Atlantic, “but the inability to cope with the experience.” Romme’s colleague, Dr. Dirk Corstens, also believes we must limit the medication prescribed for patients with psychosis because it often does more harm than good.
2A Dispute About Chemical Imbalance
Drugs to treat psychosis are some of the best-selling medications in the US. However, evidence continues to show that these drugs are not treating a chemical imbalance that causes mental illness. In fact, the first drugs prescribed for mental illness—Thorazine, Miltown, and Marsilid—were actually developed to combat infections. When they were found to quiet mental symptoms, researchers observed that they also affected brain chemistry. The drugs weren’t created to treat abnormal brain chemistry. The theory of chemical imbalance was created to explain the use of the drugs. Decades of additional research have failed to confirm the chemical imbalance hypothesis with different classes of drugs to treat mental illness.
Even so, the more important question is whether the drugs work. By reviewing the published results of clinical trials to treat depression, Irving Kirsch, a UK psychologist, initially found that placebos worked about 82 percent as well as antidepressant medications. But his most important finding was that drug companies can bury the results of tests they don’t like. So they can keep testing until they get the results they want to publicize. Kirsch concluded that the drugs showed no significant clinical difference than placebos in treatment. Even though there was a small statistical difference, it just wasn’t enough to matter in terms of actual treatment.
He also found that drugs that weren’t antidepressants—such as sedatives, thyroid hormones, stimulants, opiates, and even certain herbal remedies—did just as good a job in relieving depression symptoms as antidepressants. When he looked at high doses of placebos that had side effects, he observed the same results. So he concluded that the presence of side effects may make patients believe that drugs are doing a better job for them than placebos without side effects.
Kirsch’s study is just one review of a complex topic, and no one should decline medication because of it. But it raises questions about the efficacy of medication, and others should conduct further research on the subject.
1The Eventual Fading Away Of Our Delusions
In Western society, we’re often convinced that our scientific approach to mental illness makes us more sophisticated than the mental health practitioners from other cultures and times. This arrogance leads us to look at earlier treatments with a mixture of ridicule and sadness.
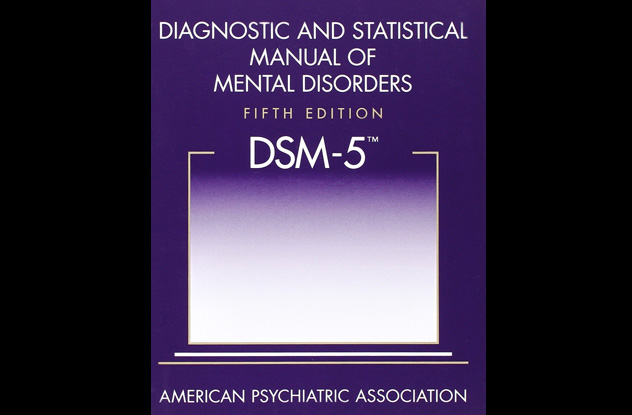
We now have the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM), known as the “Bible of psychiatry.” It lists symptoms of disorders that are considered to be psychiatric illnesses in the US. So, in a way, it defines what our society views as normal and abnormal behavior—what can let us roam free and what can put us on medication or even get us locked up.
However, the DSM isn’t as objective as we’d like to believe. US psychiatrist Daniel Carlat explains that psychiatrists have received the most money from drug companies for many years because “our diagnoses are subjective and expandable, and we have few rational reasons for choosing one treatment over another.” Carlat also says that he makes 80 percent more per hour by prescribing drugs rather than talk therapy, so he only prescribes drugs.
“Patients often view psychiatrists as wizards of neurotransmitters,” he says, “who can choose just the right medication for whatever chemical imbalance is at play. This exaggerated conception of our capabilities has been encouraged by drug companies, by psychiatrists ourselves, and by our patients’ understandable hopes for cures.”
Psychiatrists ask patients about their symptoms to see if they match any conditions in the DSM. The more matches, the more drugs that may be prescribed. It’s a way of labeling patients that makes us feel cared for and makes money for the medical community. But according to Carlat, that doesn’t necessarily mean he has any idea what he’s doing.
If that’s the way our culture is defining delusions, we can only hope they will fade away sooner rather than later. It also raises the question of how future generations will view our delusions and the doctors who treated them.