 Weird Stuff
Weird Stuff  Weird Stuff
Weird Stuff  Mysteries
Mysteries 10 Tragic Disappearances and Deaths in Joshua Tree National Park
 History
History 10 Ways Childhood Really Sucked in the Old West
 Music
Music 10 Name Origins of Famous Bands from the 1990s
 Religion
Religion 10 Biggest Turnarounds by the Catholic Church
 Weird Stuff
Weird Stuff 10 Unbelievable Times Laws Had Unintended Consequences
 Humans
Humans Ten Historic Women Who Deserve Way More Credit Than They Got
 Movies and TV
Movies and TV 10 Films That Spawned Major Lawsuits
 History
History Ten Times Towns Were Wiped Off the Face of the Earth
 Creepy
Creepy 10 of the Most Disturbingly Haunted Public Houses in the UK
 Weird Stuff
Weird Stuff 10 Niche Subcultures That Are More Popular Than You Might Think
 Mysteries
Mysteries 10 Tragic Disappearances and Deaths in Joshua Tree National Park
 History
History 10 Ways Childhood Really Sucked in the Old West
Who's Behind Listverse?

Jamie Frater
Head Editor
Jamie founded Listverse due to an insatiable desire to share fascinating, obscure, and bizarre facts. He has been a guest speaker on numerous national radio and television stations and is a five time published author.
More About Us Music
Music 10 Name Origins of Famous Bands from the 1990s
 Religion
Religion 10 Biggest Turnarounds by the Catholic Church
 Weird Stuff
Weird Stuff 10 Unbelievable Times Laws Had Unintended Consequences
 Humans
Humans Ten Historic Women Who Deserve Way More Credit Than They Got
 Movies and TV
Movies and TV 10 Films That Spawned Major Lawsuits
 History
History Ten Times Towns Were Wiped Off the Face of the Earth
 Creepy
Creepy 10 of the Most Disturbingly Haunted Public Houses in the UK
10 Bacterial Candidates For Bioweaponry
Nuclear weapons, although still disastrous and powerful, are a thing of yesteryear. Now, a new type of weapon is growing in popularity. This is exemplified by the increasing number of books, movies, and video games featuring zombies, viral attacks, and fungal weapons. In many of these stories, biological catastrophes always lead to a dystopian future, and these fictional worlds represent a terrifying reality. Bioweapons are the next big thing.
10 Bacillus Anthracis

Among all bacterial bioweapons, there is probably nothing more popular than Bacillus anthracis, the pathogen used in an infamous attack code-named “Amerithrax” by the FBI. In the days following 9/11, several letters containing B. anthracis spores were sent to news media offices and two US senators. Five people were killed in the attack while 17 developed anthrax symptoms. With 10,000 witnesses having participated in the investigation, this was one of the most extensive biological cases in US history.
B. anthracis is a very potent pathogen. In fact, it is an obligate pathogen by nature. This means that acquiring it will almost always lead to disease. To be infected by the bacteria, the victim must ingest the spores. Spores are the dormant derivative of many bacilli bacteria. They are resistant to extreme environmental conditions such as heat, dehydration, and disinfectants. B. anthracis causes anthrax, which manifests in different forms such as blisters, necrosis, abdominal pain, diarrhea, headache, and many more unpleasant symptoms. If left untreated, death usually follows.
B. anthracis is a good candidate for a bioweapon due to its spores, which are very economical for transmission and stockpiling. Additionally, it causes anthrax by producing different toxins leading to high mortality. However, B. anthracis is not transmissible by person-to-person contact, thus limiting the spread of anthrax attacks. Also, there is a growing trend of vaccine development against anthrax.
9 Brucella
 Brucella is a zoonotic pathogen, normally residing in animals. When transferred to humans, it causes a disease called brucellosis. Normally, it is spread from animals to humans via consumption of contaminated foods, especially unpasteurized dairy products. It may also enter the body through wounds. Hence, personnel working closely with animals—think veterinarians, food processing plant employees, slaughterhouse workers, etc.—are highly vulnerable.
Brucella is a zoonotic pathogen, normally residing in animals. When transferred to humans, it causes a disease called brucellosis. Normally, it is spread from animals to humans via consumption of contaminated foods, especially unpasteurized dairy products. It may also enter the body through wounds. Hence, personnel working closely with animals—think veterinarians, food processing plant employees, slaughterhouse workers, etc.—are highly vulnerable.
Brucella is a good bioweapon candidate as it can also infect humans via inhalation of contaminated dust or aerosol. Such airborne pathways can make way for large-scale infection. Infected individuals may experience repeating (undulating) fever, pain, headache, swelling of the genitals, liver failure, and arthritis. Lethal manifestations occur when complications develop, with cardiac-related ones such as endocarditis usually leading to death.
Potential cases of indirect Brucella attack include feeding Brucella-infected carcasses to cattle, which is what happened in the UK back in 2011. Brucella can rarely be transmitted via person-to-person contact, and live cells must be inhaled or contacted for infection to occur . . . which makes deliberate transmission a little bit problematic. However, since it takes about two to four weeks after initial contact for symptoms to occur, transmission may go unnoticed for a period of time before diseases sprout out.
8 Francisella Tularensis
 Francisella tularensis is categorized as Tier 1 by the US government. In other words, the bacterium is highly weaponizable and may cause severe threat to humans. It causes tularemia and infects both humans and a variety of animals. A person can be infected in a great number of ways. For example, touching infected animals (like hares) is quite dangerous, as is coming into contact with mucosal skin (like the eye). A person can also be infected from tick bites, contact with contaminated surfaces, or by ingesting contaminated food or water. Moreover, it can also be acquired by inhaling contaminated dust particles and aerosols, making it a suitable bioweapon. Plus, it can survive in non-host environments and contaminate drinking water and food.
Francisella tularensis is categorized as Tier 1 by the US government. In other words, the bacterium is highly weaponizable and may cause severe threat to humans. It causes tularemia and infects both humans and a variety of animals. A person can be infected in a great number of ways. For example, touching infected animals (like hares) is quite dangerous, as is coming into contact with mucosal skin (like the eye). A person can also be infected from tick bites, contact with contaminated surfaces, or by ingesting contaminated food or water. Moreover, it can also be acquired by inhaling contaminated dust particles and aerosols, making it a suitable bioweapon. Plus, it can survive in non-host environments and contaminate drinking water and food.
The manifestation of the disease depends on the location of the infection. But generally, victims will suffer from symptoms such as skin lesions, fever, swelling of lymph nodes, and inflammation of the eye. Pneumonic tularemia is the most severe and lethal among all variations. If treatment is delayed, death can follow the infection.
7 Clostridium Botulinum

Botulism is caused by Clostridium botulinum, a common soil bacterium that, like Bacillus anthracis, can produce dormant spores. It is a paralytic disease caused by a neurotoxin produced by the bacterium. The toxin is very potent and can cause a mortality rate of up to 50%, although the casualties have dropped significantly in recent years.
The most probable route for a weaponized Clostridium botulim would be through ingestion of spores in contaminated food products. Since the spores are highly resistant to stress, they can survive many types of food processing methods, including heat treatments, chemical treatments, and even canning. After the spores successfully enter the body, the bacteria will grow and produce the neurotoxin botulinum, thus paralyzing the victim. If the respiratory organs are paralyzed and fail, death is likely to follow. Otherwise, the infected person will require a mechanical breathing apparatus.
6 Yersinia Pestis

Yersinia pestis is the causative agent behind the infamous Black Death, the plague that ravaged Europe as early as the 14th century. Normally, the bacteria resides in rodents and fleas. However, humans can become infected if bitten by the fleas or by handling diseased animals.
Once infected, the plague can develop into three varieties. Bubonic plague will manifest as buboes, which are painful and swollen lymph nodes. If left untreated, it can then develop into septicemic plague, which can cause organ damage and internal hemorrhaging. Another form is pneumonic plague, which may lead to respiratory problems.
The plague can be transferred from one person to another by inhaling contaminated respiratory droplets, such as those caused by sneezing. Therefore, pneumonic plague is most suitable for biological attacks. However, the use of Yersinia pestis has a few disadvantages. For airborne transmission to occur, potential targets must be physically close to each other or else the contaminated droplets will not reach their victims. Also, if the infection is treated early, mortality can be avoided simply by using readily available antibiotics.
5 Leptospira
Leptospira is a group of spiral-shaped bacteria that reside in different kinds of animals, especially rodents. It causes leptospirosis, which can develop into a severe infection known as Weil’s disease. A person can become infected with Leptospira when animal urine containing the pathogen comes into contact with open wounds. Contaminated animal urine may also get into water supplies and infect large numbers of people.
Leptospirosis can manifest itself in symptoms such as muscle ache, vomiting, abdominal pain, diarrhea, rash, and fever. In many cases, it may cause liver failure, which can be detected by the yellowing of the skin. This condition is also called jaundice. The infection may also result in respiratory problems and internal bleeding, often causing the victim to cough up blood. Fortunately, the infection can be treated with penicillin.
If used as a bioweapon, it’s likely that Leptospira will be used to contaminate drinking water. In such an environment, the bacterium can survive for long periods of time.
4 Pasteurella Multocida
 Pasteurella multocida was named after Louis Pasteur, one of the founding fathers of microbiology. It was first discovered in birds infected with cholera. The bacteria is common to many animals, including house pets like cats and dogs. A person can be infected through animal bites and scratches.
Pasteurella multocida was named after Louis Pasteur, one of the founding fathers of microbiology. It was first discovered in birds infected with cholera. The bacteria is common to many animals, including house pets like cats and dogs. A person can be infected through animal bites and scratches.
When transferred to humans, P. multocida can cause cellulitis, an infection of the skin. If it crosses the blood-brain barrier, it may manifest as meningitis. The bacterium may also reside in the blood and can cause endocarditis, the infection of heart valves. If it progresses further, cardiac problems may lead to mortality.
Although animal contact is the best known way to acquire P. multocida, contact with contaminated nasal liquids can also be quite dangerous. Therefore, close interaction with infected persons is not advised.
Using P. multocida as a bioweapon can be a pretty big hassle. First, options for transmission are extremely limited. Second, it’s easily treated by readily available antibiotics. Lastly, while the disease can cause severe problems, there’s a chance it might only result in mild symptoms.
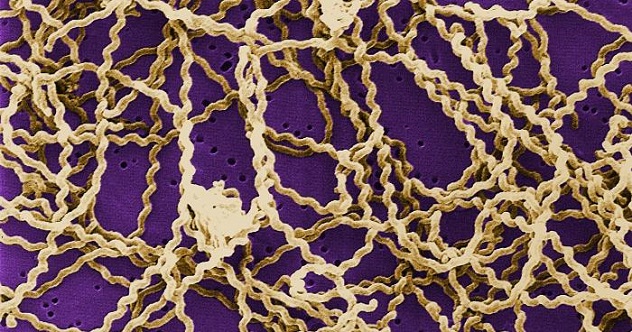
3 Borrelia Burgdorferi

Borrelia burgdorferi causes borreliosis, an illness better known as Lyme disease. The bacterium is transmitted to humans when a deer tick, scientifically known as Ixodes scapularis, ingests contaminated animal blood and then passes the pathogen to a human host. Infection commonly manifests as fever, headache, swelling of lymph nodes, and chills.
However, the most distinguishing symptom of Lyme disease is the presence of rashes. This almost always gives the disease away. Furthermore, late symptoms may include facial palsy or the loss of facial muscle tone, thus leading to disfigurement, irregular heartbeat, and pain. The pathogen may also infect the nervous system, leading to inflammation of the brain.
If the bacterium enters the bloodstream and infects the heart, the resulting disease is called Lyme carditis. This can be fatal if the heart malfunctions and fails.
Severe manifestations and complications can be prevented if the disease is detected early. Therefore, although a potent bioweapon candidate, there are sufficient methods to thwart such attacks.
2 Coxiella Burnetii
Coxiella burnetii is a very small bacterium normally residing in cattle, sheep, and goats. It causes the disease called Q fever. Transmission is commonly the result of handling infected animals. However, since the bacterium can be passed on through the milk of dairy animals, consumption of unpasteurized or improperly treated milk is equally dangerous. The pathogen can also be spread by air transmission and person-to-person contact.
C. burnetii is a significant problem among food processing companies. Since it can develop dormant spores, it is highly resistant to heat and chemical treatments. Therefore, foodborne infections are very possible. Once infected, a person may develop symptoms such as fever, pains, chills, vomiting, and diarrhea. However, it may also manifest as hepatitis, myocarditis, pneumonia, and meningoencephalitis. The bacterium may also cause chronic infections, with symptoms occurring years after initial contact.
Although airborne, C. burnetii has one major drawback as a potential bioweapon. As it turns out, infected individuals might never develop symptoms.
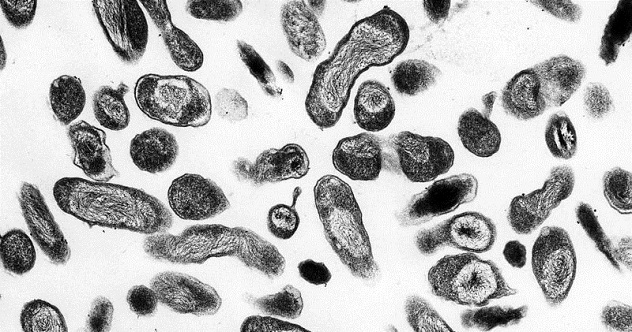
1 Rickettsia
 Rickettsia is a diverse group of closely related bacteria that are responsible for a variety of diseases. These diseases include illnesses like rickettsialpox and both murine and epidemic typhus. However, the most common of all is Rocky Mountain spotted fever, abbreviated as RMSF. The disease is transmitted through tick bites, especially by the American dog tick, the Rocky Mountain wood tick, and the brown dog tick.
Rickettsia is a diverse group of closely related bacteria that are responsible for a variety of diseases. These diseases include illnesses like rickettsialpox and both murine and epidemic typhus. However, the most common of all is Rocky Mountain spotted fever, abbreviated as RMSF. The disease is transmitted through tick bites, especially by the American dog tick, the Rocky Mountain wood tick, and the brown dog tick.
The disease can prove fatal if not treated early. Early symptoms include fever, headache, vomiting, abdominal pain, and nausea. The illness’s characteristic rash develops at least two days after the onset of fever. As a result, early diagnosis may miss the disease. In such a scenario, successful treatment may no longer be attainable as early diagnosis and treatment are vital. This concept is useful for bioweaponry as misdiagnoses are common, thus leading to high mortality.
However, if it’s caught early and treated promptly, fatal complications may be averted.
Matthew is a pre-medical student majoring in microbiology.