Our World
Our World  Our World
Our World  Technology
Technology 10 Most Devastating Computer Viruses
 Miscellaneous
Miscellaneous 10 Allegories That Imagine if Countries Were People
 History
History 10 Times Governments Banned Colors for Bizarre Reasons
 Health
Health 10 Terrible New Health Findings
 Weird Stuff
Weird Stuff The 10 Biggest Celebrity Death Hoaxes Ever
 Miscellaneous
Miscellaneous 10 Fascinating and Unexpected Uses of Poetry from History
 Movies and TV
Movies and TV 10 Horror Films That Failed to Launch Their Franchise
 Animals
Animals Ten Animals That Are More Musical Than You Might Think
 Technology
Technology 10 Human Inventions That Are Rewriting the Future
 Our World
Our World 10 Times Cities Tried to Reinvent Themselves and Failed
 Technology
Technology 10 Most Devastating Computer Viruses
 Miscellaneous
Miscellaneous 10 Allegories That Imagine if Countries Were People
Who's Behind Listverse?

Jamie Frater
Head Editor
Jamie founded Listverse due to an insatiable desire to share fascinating, obscure, and bizarre facts. He has been a guest speaker on numerous national radio and television stations and is a five time published author.
More About Us History
History 10 Times Governments Banned Colors for Bizarre Reasons
 Health
Health 10 Terrible New Health Findings
 Weird Stuff
Weird Stuff The 10 Biggest Celebrity Death Hoaxes Ever
 Miscellaneous
Miscellaneous 10 Fascinating and Unexpected Uses of Poetry from History
 Movies and TV
Movies and TV 10 Horror Films That Failed to Launch Their Franchise
 Animals
Animals Ten Animals That Are More Musical Than You Might Think
 Technology
Technology 10 Human Inventions That Are Rewriting the Future
10 People Who Have Improved Western Medicine
We take a lot for granted in terms of medical care today. Whilst we still get ill sometimes, there is a range of medicines and treatments available. Our doctors have a huge body of knowledge and experience to call upon, and we can usually rely on having modern and clean facilities. It wasn’t always like this. This list is in honor of all of the people who have improved the knowledge and practice of medicine.
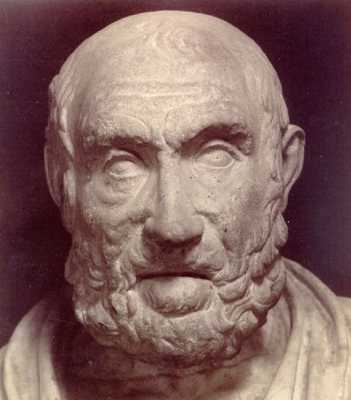
Hippocrates was a physician in Ancient Greece. He is thought by many to be the Father of Western Medicine. He was an incredibly forward thinking man who developed ideas that were ahead of his time. He was outspoken in his belief that illness was not caused by the displeasure of the gods, but had actual physical causes. He acknowledged that lifestyle, diet and environmental factors all affected physical health. It sounds obvious to us now, but that is because we have over 2,000 years of his influence to thank. At the time this was an incredible belief, that questioned both the authority of the gods, and other physicians of the time.
At this point in history people did not understand the internal workings of the human body in the same way that we do now. It was a great taboo to dissect the dead, so the nervous and circulatory systems had not been studied. The accepted theory of was that illness was caused by the four “humors” or different types of fluid that inhabited the body being out of balance. All treatments were prescribed on this assumption, and Hippocrates himself believed this.
Hippocrates treated patients and taught his knowledge to others. He had a dedicated following of people around him, who helped treat others according to his principles and thus increased his renown. He is credited with writing the Hippocratic Corpus. This is a collection of over 70 documents which describe the symptoms, and progression of diseases. This has been passed down over the millennia since his death, and has informed medical practice right up to the present day.
He believed in the importance of observing the patient to see the progression and development of symptoms, and to review how effective the treatment was in combating these. He was also a founder in the practice of taking medical and family histories from patients. These are routine practices for any medic today, but they originated with Hippocrates.
Hippocrates is probably best known as the creator of the Hippocratic Oath. This is a statement of moral and professional ethical standards that physicians were expected to abide by. This is still sworn on graduating medical school in some areas (in an updated form).

Florence Nightingale is possibly the most famous nurse in history, she is known as “the Lady with the Lamp”. The facts that are known about her are often shrouded in exaggeration and legend.
She was born to an upper class British family, and was highly educated. She felt that she was called by God to become a nurse; a move which her family felt was beneath her. She went to the Crimean front in Eastern Europe to tend to soldiers in 1854, where hospitals had an appallingly high death rate. At the time diseases such as cholera and typhoid fever were rife, with soldiers being seven times more likely to die after admission to hospital than they were on the battlefield. The importance of sanitation was not fully understood at the time, and patients were housed in dirty conditions, surrounded by the human waste of those with infectious diseases. It is widely thought that she improved the hygiene conditions in the hospital during the war, causing the death rate to drop. This is not accurate, or a claim that she ever made. In fact the British government sent the sanitation commission to the area. They cleaned the sewage out of the military hospitals, after which the mortality rates dropped.
Nightingale was a talented mathematician, with a passion for statistical analysis. She was the first female member of the Royal Statistical Society. Following her return from the Crimea she did analysis into the rate of death and what had affected it, and found statistical evidence that it was the improvement of sanitation and cleanliness that had made the biggest changes in improving the survival rates. She used the irrefutable statistical data to lobby politicians and influential committee members, persuading them to make major changes to the hospital systems, both at home and for the military.
She set up a nurse training college in St Thomas’ Hospital in London in 1860. Prior to this, nurses had a poor reputation of being rough and crude women with little training, loose morals and regular drunkenness. It was not considered a suitable profession for well brought up ladies. Nightingale schools had strict regulations about behavior and sobriety, and had a curriculum for student nurses to follow. They also emphasized the importance of clinical training on wards. Nightingale herself continued to write textbooks of nurse education. International Nurses Day is still celebrated on her birthday every year, 12th of May.
The changes that she influenced in healthcare caused a major transformation in patient care and nurse training. These have had a major impact on the way that medical care is given today, and it is this level of influence that has set her apart from other nurse innovators of the time.
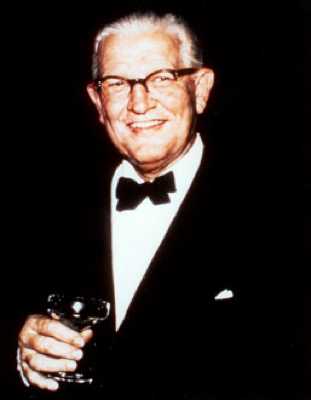
Archibald McIndoe was a doctor from New Zealand. In 1938 he was made the consultant plastic surgeon to the RAF. When the Second World War started he found himself treating pilots who had been shot down during military action. They were often horrendously burnt due to the aviation fuel igniting. Reconstructive plastic surgery was still in its infancy, and McIndoe was one of only four plastic surgeons in the UK at the time.
The conventional methods of using acid to remove damaged skin and then waiting two months before trying to perform surgery meant that the pilots had to spend long periods in agony. It also resulted in a great deal of scar tissue. McIndoe decided to operate immediately, cutting away damaged tissue so that skin grafts could be placed straight away. This greatly increased the chances of healing, resulting in less scarring and much more mobility. He also developed new skin graft techniques which resulted in lower infection rates and more successful grafts. The men who were in his care became known as The Guinea Pig Club as the methods McIndoe tried were so ground-breaking.
It is not just the pioneering physical care that McIndoe gave which marks him as an exceptional man. He also recognized the incredible value of psychological rehabilitation for the servicemen who were in his care. It was usual for burn victims who had disfiguring injuries to shun the public eye. He felt that it was important for them to remain part of their community, and to have pride in what they had done for their countries. Many of the men were in hospital for a number of years, having multiple reconstructive surgeries, and so their local community became East Grinstead, where the burns unit was. He encouraged them to wear their service uniforms instead of hospital gowns, to maintain their professional pride, and he encouraged the community to engage with and support them. It became an honor to have them over to their homes, and they attended film openings and events. This side of McIndoe’s legacy has been slow to catch on, but people are now realizing the importance of maintaining support and integration for those who have been injured.
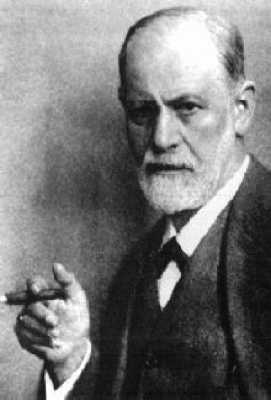
Freud was an Austrian neurologist and psychiatrist, although he is better known as the Father of Psychoanalysis. He treated patients with “hysterical” illnesses and neurosis. At the time society, including the medical establishment was incredibly sexist. The majority of Freud’s patients were women suffering from hysterical illnesses and neurosis. This included female “willfulness”. Although there are still a higher proportion of women that suffer from anxiety related symptoms than men, the treatments for them at the time could be extreme. One popular treatment was the use of an “electrical vibrator” to stimulate orgasm, as this was felt to be a cause of hysteria. Bear in mind that not all of these women will have been treated willingly, particularly those in the asylums of the time. This left many women in a position where they were treated for willfulness and anxiety by medically sanctioned rape. Other treatments include applying dung to the genitals, leeches, arsenic treatment, and surgical destruction of the clitoris.
Freud felt that these treatments were not effective, and failed to address the root of the problem. He was one of the first to consider that these illnesses may have a psychological, rather than physical cause. He developed a treatment which was unheard of at the time, which basically involved listening to the patient. He was a pioneer of the “Talking Cure”. He initially tried hypnosis, and later used his method of psychoanalysis. This involves exploring the symbolic meaning of the patients’ symptoms and memories to try to identify repressed memories. He felt that if they could be confronted the troubling symptoms would stop. Freud was one of the first people to scientifically acknowledge that “hysterical” illnesses could be due to traumatic memories which were repressed.
Freud also developed theories about sexuality, and stated that the development of a healthy functioning person was due to successful transition through stages of sexual development. He gave us the idea of the Oedipus complex. This is where a male child sees his mother as his main focus and falls in love with her. He feels threatened by the presence and dominance of the father and worries that he may be castrated. He described a similar phase in females, where the focus is on the father, and he describes penis envy, stating that women feel incomplete due to the lack of this appendage. He also described the oral, anal and phallic stages of childhood development, where the primary sexual urge is related to each of these three areas in turn. Freud felt that problems in progressing through these stages were the main cause of neurosis and anxiety in adults. His focus on symbolism of dreams and conversation led to the term “Freudian Slip” being coined, to mean an error in speech which is symbolic of our true desires or meaning.
Although many people feel that Freud’s theories overvalue sex, he also had a societal impact in bringing the subject of sex and individual sexuality to the forefront. It is important to remember that when Freud was developing his theories, sex was not discussed in the way it is now, and Victorian values reigned. Although Freud’s theories were made from a male perspective and have been widely criticized by feminists, he himself acknowledged that the female perspective needed further investigation.
Currently psychoanalysis is in decline, and is not widely used as a treatment. It is, however, the precursor for modern psychological treatment. The vast majority of treatment of anxiety based disorders is now with verbal therapy, allowing people to discuss and explore their problems and the reasons for them. Prior to Freud this would have been impossible. He has allowed the area of psychology and the related area of psychiatry to advance dramatically. His theories have become widely known outside of the medical field, and have encouraged the consideration of psychology to become popular. This has made a huge impact in helping to reduce the stigma of mental illness.

Marie Curie was a Polish born scientist, although she moved to France to study and stayed there after meeting her husband. She researched and experimented with radioactive substances, and invented the word “radioactivity”. Her husband, also a scientist, assisted with her research and in 1903 they were both awarded the Nobel Prize in physics for their research into the “radiation phenomenon”. Curie is the discoverer of both Radium and Polonium and in 1911 she was awarded the Nobel Prize for chemistry for her discoveries. She was the first women to be awarded a Nobel Prize, and was the first person to win multiple Nobel Prizes. She remains the only woman to have won the award twice. At the time much of the French government and scientific establishment were very negative towards her because of her gender, refusing to acknowledge a female scientist among their ranks.
Curie’s research helped to develop radiation as a therapeutic tool. Curie’s research identified that it can do localized damage to a targeted area of the body, and could be useful in treating cancerous tissue. This is still the foundation of radiotherapy today, although the methods have changed. At the time she filled small glass tubes with Radon (a radioactive gas) that could be inserted into the area of the tumor, causing it to shrink.
During World War One, Curie and her daughter used their findings to help soldiers injured on the front lines. They fitted x-ray machines to vehicles and drove them directly to field hospitals. They were able to show the location of bullets, shrapnel or broken bones, and were a great assistance in providing appropriate medical care.
Unfortunately, at the time the harmful effects of working with radioactive materials were not known, and both Curie and her husband suffered ill health due to their high levels of exposure. They both exhibited sores on their fingers from handling the materials directly, and Curie herself eventually died of leukemia. Her research notebooks have such high levels of radioactivity that it is still not safe to handle them without protective equipment. Belatedly, the French government ensured that both of the Curie’s remains are now at the Panthéon in Paris. She is currently the only woman to be there on her own merit. The effect of radiotherapy, and later chemotherapy, and on-going research into cancer and leukemia cannot be overestimated. The result of Curie’s work has saved countless lives.
Blundell was a British obstetrician. At the time it was common for women to die in childbirth. He wondered if women who bled heavily after giving birth (and usually died) may be able to be given someone else’s blood. He experimented to find a way to safely transfuse blood from one person to another. He invented equipment specifically for this purpose, some of which is still in use today.
Prior to this, people had experimented with orally feeding blood to another person but this had been unsuccessful. Experiments were also made giving the blood of animals to humans. Some survived, although it appears that this was due to only receiving such small amounts of the blood that they only had a minor allergic response. Blundell identified that for a human to successfully receive a blood transfusion of any significant quantity and survive, it needed to be from a human. He identified that blood that was stored would coagulate and realized that for his work to be successful the transfusions needed to be made on site. He eventually performed the first successful human blood transfusion from a husband to his wife when she started to hemorrhage following the birth of their child.
Not all of Blundell’s patients survived, but at the time they were also not aware of blood typing and the problem of immune rejection. Research into this was done later and further innovations have been made in this field, but Blundell should be acknowledged for pioneering the human blood transfusion. In the UK alone there are currently 8,000 units of blood used daily, and the World Health Organization reports that in 2007, 85.4 million units were collected. Transfusions save the lives of millions. Whether through accident, surgery, or chronic illness, people survive today who otherwise would not have.

Joseph Lister was a British surgeon and professor of surgery. He is known as the Father of Asepsis. At the time people did not understand that germs exist, and how many illnesses are carried through the transfer of infected particles. They thought that illness was spread by miasmas (bad air), and used fragrant herbs and flowers as a way of warding off disease. Lister noticed that many of the people he operated on survived the surgery, but later died from what were known as “ward fevers”. In fact the rate of death from post-operative infection at the time was huge.
Around this time the first research was being done into microorganisms, and Lister was aware of this. He proposed that the reason for post-operative infection was that organisms were flourishing in the wounds. He noted that doctors often went from one surgery to another without washing their hands, dealing with infected tissue before doing an invasive procedure on another patient and introducing the infection into the wound.
He decided to try using carbolic acid as a disinfectant. He encouraged his surgeons to wash their hands in a solution of it prior to surgery, and to wear clean gloves. He also used it on his surgical equipment, had assistants spray a solution of it in the operating theater during surgery and used it to clean wounds and dressings. The rate of infection fell dramatically following the implication of these measures, and Lister was able to influence others at the time to acknowledge his techniques.
Lister’s findings are still relevant today. This is the point at which improvements in sterilization and asepsis started, and this is important to consider in the age of MRSA and other hospital acquired infections.
Joseph Murray was originally a plastic surgeon. He operated on injured WWII servicemen. He was regularly using skin grafts to repair injured tissue, and became interested in the phenomenon of tissue rejection. At the time, research was being done which showed that there was an immune response which caused rejection. He wondered whether there was a way to overcome this and began his own research into rejection of tissue and organs.
He decided to look at the possibility of a kidney transplant. At the time a person with kidney failure would not have had much of a chance. An attempt had been made by a Ukrainian surgeon in the 1930s to transplant a kidney, but the patient had died because of the immune system rejecting the new organ. They needed to find a way to see if the operation could be done without the immune system rejecting the new organ. In 1954 Richard Herrick needed a new kidney, and his identical twin brother Ronald offered his. As the tissue of each twin was identical, the immune response should be avoided. Murray and his team operated on the Herrick brothers, successfully transplanting a kidney with no rejection. It was the first successful human organ transplant.
Murray continued his work in transplantation, later performing the first transplant from an unrelated person with immunosuppressant drugs. In 1990 Murray was honored, along with E. Donnall Thomas, with a Nobel Prize for medicine for their work in organ and cell transplantation.
Alexander Fleming was a renowned biologist and pharmacologist. He is also known as the Father of Antibiotics. He is credited with the clinical discovery of Penicillin. This was an accidental discovery. Fleming had a messy lab, and had forgotten to put away all of the influenza samples he had been working on before going on holiday. On his return he found that mould had grown on some of the infected petri dishes. Where this mould had come into contact with the influenza cultures, it had been destroyed. Fleming did further research into this unexpected mould and found that it could safely be given without observing any ill effects (the allergy reactions that are sometimes seen were not noted in these tests). However, he found that it was very difficult to obtain enough of the penicillin to be effective, and found that growing it on a larger scale was very difficult and time consuming, so he did not progress any further with it.
Ten years later his research was continued by Howard Florey and Ernst Chain at Oxford University. They found a method of mass producing Penicillin, and in 1944, after clinical trials, obtained funding from the US and UK governments to produce it on an industrial scale. Both governments were very keen to have this “wonder drug” available to troops fighting in occupied Europe, and at risk of infection from battle wounds. In 1945 Fleming, Florey and Chain were awarded the Nobel Prize for medicine for the discovery and production of Penicillin.
Prior to the discovery of antibiotics as we know them today, there were few effective treatments for infection. Even a minor wound could become the site of a major infection that killed the patient. Arsenic and other damaging and toxic substances were used, but they caused further damage to the body. People died en mass of influenza epidemics, tuberculosis, scarlet fever, meningitis, pneumonia, and diphtheria. Gonorrhoea and syphilis were common sexually transmitted diseases. All of these diseases can be fatal, and if they are survived, can cause an incredible amount of chronic damage. The discovery of Penicillin and the development of new antibiotics over the years have allowed us to treat illnesses that blighted humanity for millennia. They can still be serious if they are caught, but now people have a chance of survival that our ancestors did not have.

Edward Jenner was a British doctor. He is considered to be the Father of Immunology. At the time there was no preventative medicine in the form that would be recognized today. There was no vaccination against illness, and epidemic was rife, devastating whole communities. Smallpox was a particularly virulent disease which was thought to have been contracted by around 60% of the population of countries where it was endemic, killing around 20%. This wiped out whole communities, leaving millions dead every year. There was, and still is, no known cure for smallpox, so the only hope is not to catch it. It is the disease responsible for devastating the Native American, Incan and Aztec populations when colonized by Europeans. It was no respecter of age or rank, wiping out royalty and common people alike. It results in fever, and a rash which transforms into fluid filled pustules. People who caught it were not expected to survive, and those who did were scarred for life by the pustules. Survivors were also often left blind. People were so scared of this disease that they tried to inoculate themselves against it by inhaling the scabs from smallpox sores. Unfortunately, this often lead to the person contracting the full blown disease.
In the midst of this, Jenner noted that milkmaids who frequently caught a less extreme version of the illness called cowpox, never seemed to catch smallpox. Cowpox caused blisters on the skin, similar to smallpox, but was not fatal. He theorized that cowpox might give the person immunity to smallpox and, amazingly, managed to get a local farmer to allow him to try an experiment on his son, James Phipps. In 1798, he drained some pus out of the blisters of a milkmaid with cowpox, and injected it into the arm of Phipps, and repeated this over a few days. He then injected him with smallpox. Phipps became unwell, but did not develop full blown smallpox and recovered within a few days with no scarring or other ill effects.
Jenner began vaccinating locals, and always offered his vaccine for free. He was adamant that he did not want it to only be available to the rich. He persevered to get his ideas accepted as there was a lot of defiance, particularly from the church, who felt that it went against God to give diseased animal material to humans. As the number of people who had been vaccinated increased the immunity became evident, with people who were protected failing to catch smallpox. His theories were accepted and within 30 years it was made compulsory to have the vaccination in England and Wales, and it was provided free to all.
Smallpox is now a non-existent illness, having been declared extinct by the World Health Organization in 1980. This was after a concerted and worldwide vaccination policy. This virulent and deadly disease has been wiped out, following work that was started by one man. However, it is not just smallpox that has been affected. Routine vaccination for major infectious illness has drastically reduced the number of cases of measles, rubella, diphtheria, tetanus, mumps, polio and meningitis C. All of these diseases are potentially fatal, and cause chronic and devastating effects in those who survive them. Jenner’s work has given us the ability to protect ourselves against contracting them. He is considered to have been ultimately responsible for saving more lives than any other person in history.